
Repetitive Blast Exposure and Mental Health:
The Challenges for Military Veterans
By Bruce Parkman
Foundation Note: The following information is recommended for Veterans to consider for further evaluation of the effects of past RBE on their brain and mental health and should not be used for self-diagnosis. A diagnosis of the impact of RBE should be left to a qualified medical practitioner, and treatment protocols developed with them and other qualified professionals. Please do not try any treatment for your brain unless you have been advised on the risks and thoroughly understand them before trying them. Some of these, like plant medicines and psychedelics, could be harmful if proper preparation methods are not followed.
Repetitive Blast Exposure (RBE): An Overview
Have you ever wondered about why the suicide rate and mental health of our veterans continue to remain one of the significant challenges to military veterans? Despite hundreds of millions of dollars spent on treatment and therapy, we continue to lose 22 (estimates range as high as 42i) veterans a day, and no other issue has dominated the press and conversation amongst military leaders and politicians as the epidemic of mental illness and suicide has. If these estimates are even close, we have lost more than 13 times the number of lives to suicide or overdose than have died in combat. What have we overlooked that could be contributing to this tragedy? The answer: Repetitive Blast Exposure, or RBE.
RBE refers to the waves of pressure, usually called Blast Overpressure that result from the firing of high-caliber weaponry, indirect fire systems, explosive ordnance/breaching, artillery, and armor. These waves of pressure, which we as veterans remember pounding our bodies (and actually enjoying it), can have detrimental effects on the body, primarily the brain, producing significant changes such as alterations to cortical thickness, decreases in white matter integrity, damage to the prefrontal cortex, cognitive and behavioral challenges, and more.ii,iii Currently it is thought that the primary injury is the impact of the blast wave that moves through the brain faster than the speed of sound on the organic components of the brain.iv,v These waves are now known to negatively impact the brain, and while there are different theories around the effects of the blast wave i.e., cavitation, astroglial scarring, and/or neuroinflammation on different components of the brain, research shows that there can be no doubt that significant changes are caused by blast exposure.vi Due to the lack of symptoms that occur in a soldier experiencing RBE through training and combat, it is now understood that these changes, incurred through long periods of intense exposure, cause changes to the brain that are known to be associated with mental illness, to include suicidal and homicidal ideation.vii
RBE is significantly different from a Traumatic Brain Injury, or TBI, which refers to an incident, like an IED, vehicle rollover, or bad parachute landing, where the brain is impacted in such a way that symptoms appear. Depending on the grade, a TBI can range from a concussion all the way to a grievous combat injury like a gunshot or blunt force trauma. Because RBE doesn’t produce symptoms, it has been assumed to be harmless for years, like its cousin Repetitive Head Impacts from contact sports, martial arts, boxing, etc. While the brain can, depending on the severity of the injury, recover and heal from a TBI, long-term exposure to RBE produces changes that are more permanent in nature. In fact, studies show that servicemembers suffer from mental illness that have been exposed to RBE that have never had a TBI, nor have been exposed to combat.viii
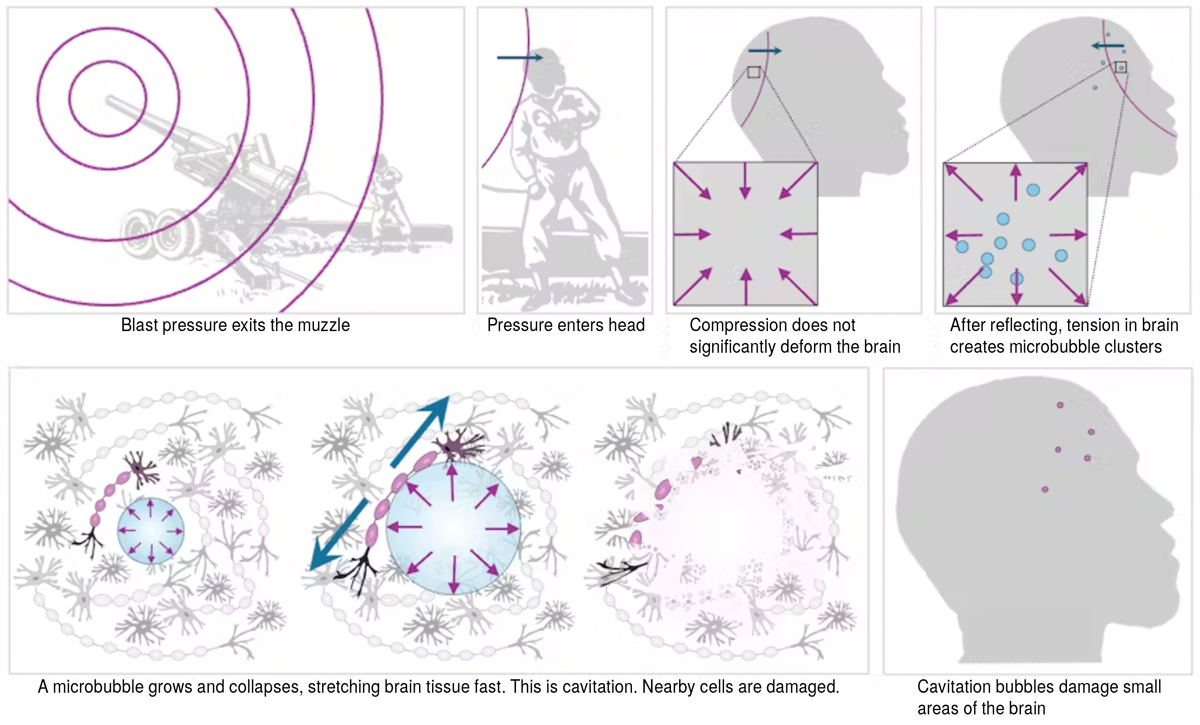
This diagram depicts how blast pressure from a gun can result in brain trauma. Alice Lux Fawzi and Manik Bansal, CC BY-NC-ND
Understanding RBE Exposure and its Impacts on the Brain and Mental Illness
So why is this now an issue? We have been in wars before; why are these veterans so vulnerable to this condition? The reason: since 9/11, the amount of exposure to RBE to the GWOT veteran is unprecedented in the history of this country due to the level, quality, and quantity of training as well as combat exposure. The GWOT veteran not only trained for combat continuously; if they were not training, they were fighting. This means that, for most of their military careers these veterans have been exposed to continuous and relentless blast exposure from weaponry, indirect fire, IEDs, explosions, and more. Unlike older veterans or older wars, the long-term exposure simply wasn’t there, whether it was from a lack of resources (post-WWI, WWII, and Vietnam) or duration of wars (Iraq 1, Grenada, and Panama).
Unfortunately, this exposure has had a significant impact on the brains, mental health and lives of our veterans and until recently, it has not been understood by the military that this was even an issue. The term blast overpressure was first acknowledged in research around 2010 and was considered fringe knowledge for years. It was not considered a risk by the military, VA or National Health Agencies as a threat; the Nation was fighting two wars, and evidence that RBE was an issue was nascent at best. As a matter of fact, until around 2018, after almost 20 years of combat and combat-related training and an unprecedented rise in mental illness among troops has the military started to focus on this issue. In the last several years, research on soldiers and RBE has provided significant evidence that this is a threat to force readiness and has resulted in changes to training and measures to reduce blast through suppression and new technologies.
While this is good news for those that have entered the military in recent years, these changes cannot impact the lives of those who entered years ago or those that have already left the military. Many of these service members have served in occupations with known elevated levels of blast exposure and multiple combat tours. With over 2M men and women that have served in Iraq and Afghanistan, many of them with years of combat and combat-related training, the numbers of affected veterans are assumed to be very high.
Limited Awareness of RBE and Its Impacts
This is compounded by the fact that RBE and its impact on the brain and contribution to the epidemic of mental illness is not a well-known subject in the medical, nursing, and psychological fields. As a matter of fact, there is minimal awareness outside of the few TBI Clinics, the NICO and other cutting-edge facilities that understand TBI and the impact of RBE on the brain. Due to the recency of this knowledge, RBE is not trained in any medical or psychological courses at this time, which means that most of the providers that the veteran may come across are not trained in this issue. In recognition of this issue, in 2023 the VA started an outreach program to contact veterans that may have been assumed to have been exposed to RBE during their careers.ix
This situation is exacerbated when it comes to mental health, as while RBE knowledge is constrained in our medical fields, the relationship between RBE and mental illness is even less recognized. There is a minimal understanding across the medical and psychological fields of the linkage between the damage to the brain that results from RBE exposure and the links from that damage to mental illness. This causes mental illness, one of the largest risks to our veteran population, to be treated as well, mental illness with no thought of the correlation between physiological damage to the brain and the resulting behavioral, psychological, and cognitive disorders. We know from countless surveys that mental illness is rampant in veteran populations; we hear about it and read about it every day, and many more are in jail (estimates range as high as 180,000 veteransx), have suffered broken marriages, lost their children, businesses, and more. There is no doubt that we have an issue with mental illness in our veteran population.
While the VA and others seem to be making great strides in improving awareness of RBE, the critical issue at hand is HOW we treat mental illness, especially considering the lack of knowledge of the link between RBE and brain damage, and this is key to understanding why change is necessary, for here is where we are failing our veterans

Marines with Combat Engineer Company detonate an oval charge and prepare to enter a building during urban mobility breaching training. (Photo by Lance Cpl. Daniel Valle, III Marine Expeditionary Force)
Current Treatments for Mental Illness Fail to Address the Impacts of RBE
For years, the standard protocols for dealing with mental illness have relied on the combined approach of therapy and pharmaceutical intervention. While this is considered “by the book” and approved by the Food and Drug Administration (FDA), this approach has not been effective in dealing with the epidemic of mental illness from a RBE perspective, particularly when we consider suicidal and homicidal ideation. The problem is that these modalities do nothing to improve the origin of the mental illness, which is a damaged brain. While pharmaceuticals are critical where suicidality, or where there is a risk of harm to self or others, the use of pharmaceuticals overall does nothing to improve brain health or healing, and for that matter, neither does therapy. In fact, when it comes to a veteran that is struggling with a mental illness that could be caused by a damaged brain, these modalities provide the veteran with little relief, as therapists, usually civilians, usually cannot relate to the veteran’s issues and the pharmaceuticals come with black box warnings (usually not disclosed) and significant side effects, which only lead to more prescriptions or exacerbate the Veterans mental health condition. It is not uncommon for veterans that have spent significant time under VA or Tricare care to have multiple medications (I have talked to Veterans with over 17 different medications) that do nothing to improve the actual health of their brain, and they have tried everything.
While the VA has taken steps to increase awareness of RBE, it is obvious that those is the area of diagnosis and treatment where significant change is needed to improve the qualitative level of care. This will require an approach to care that, regrettably, is not one that the military, or, in that case, health care, is familiar with or favorable of accepting. Unfortunately, the VA and Tricare approach to “FDA Approved” modalities bring us back to the problematic issue of pharmaceutical intervention and therapy that has not impacted our suicide rates at all. While, to the average person, it seems logical that you only need to study an issue so much to understand it. However, science and medicine want to work in terms of a definite understanding of the problem and they want “evidence-based studies” and “protocols” that can be used to diagnose and treat a condition. However, these studies take years, even decades, before treatments and protocols are approved, and while Healthcare is willing to wait on them, we cannot. TBI has been studied for well over a decade, and the standard protocols for veterans suffering from the effects are still not having a definite and scalable impact.
That is because the brain is like space, a frontier where some things are known and many things poorly, if not completely, understood. A broken brain is not like a bone; there are so many variables and conditions that there can be no guaranteed outcome of any known treatment that is provided to someone. It is so complex, with over 100,000 miles of myelin and almost 100 billion neurons all contained in a gelatinous organ that is contained in a hard bony case. In fact, despite billions of dollars spent on research and pharmaceutical development, many psychiatrists will tell you that they only have a 25% expectation that any pharmaceutical that they prescribe will work. Yes, 25%. And we want to wait another 10 to 20 years for a definite answer to treating the issue of RBE-induced mental illness? NO.
Because it’s going to take decades to deliver what the scientists want, we need to think outside the box when it comes to alternative forms of diagnosis and treatment, especially when it comes to veterans. We can no longer accept the current levels of suicidality and mental health as something we need to live with. There are novel approaches to diagnose and treat RBE-related mental illnesses that have been around for decades that are available without pharmaceutical intervention. Many of these have been used by thousands of veterans, and they have successfully improved their brain and mental health. While these treatments do not work for 100% of the veterans, there is an overall positive effect that is extremely high, much higher than the expectations for pharmaceuticals.
Additionally, there is minimal risk associated with these treatments. Unlike most SSRIs and SSNEs, and benzodiazepines that have black box warnings of depression and suicidal ideation and have been shown to be ineffective, these treatments, like electronic stimulation of the brain, Hyperbaric Oxygen Treatment, plant medicines, or supplementation programs, have minimal risk to the brains or health of veterans when conducted under the proper level of medical care. In fact, current response rates of favorable impact on the brains of veterans that have undergone treatments that we have talked to are well over 80 to 90%. Others, like Ibogaine and Ayahuasca, have shown to be absolutely critical to saving veterans’ lives who have tried all other options offered by our current military and healthcare systems.

Soldiers assigned to 1st Stryker Brigade Combat Team, 4th Infantry Division, stack up against a simulated door for a silhouette charge (U.S. Army photo by Capt. Daniel Parker)
Veterans Must Understand the Impacts of RBE and Treatment Options
So, what is a veteran to do, may you ask? First, the veteran has to be educated in several areas surrounding the issue of RBE so that they can talk to their provider about their exposure and discuss options for diagnosis and treatment.
Exposure: In the area of RBE, there are many studies out there that cover the issue; you can google RBE or Blast Overpressure to understand that the U.S. Government has spent millions of dollars on this issue and that there is a lot to read on it alone. In fact, some studies state that RBE should be a consideration when mental health issues are present.xi Suffice to say that if a veteran served in any of the following MOS’s: Tanker, Artillery, EOD, Special Forces, or Infantry where there is significant presence of RBE, the veteran should be cognizant of both the amount of time they spent in the MOS as well as the amount of time spent in combat. To provide a value to the amount of exposure a veteran may have Researchers came up with a Generalized Blast Exposure Value, or GBEV, that can be calculated by any facility that is familiar with the model. (Someone needs to create a free version of this tool.) An additional consideration is the amount of time spent in combat, as depending on the frequency of deployments, exposure and its impacts are even worse, as everyone knows that there are no restrictions in combat regarding anything, especially firing of weapons and explosions.
Diagnosis: Once it can be ascertained that there is exposure, the next step is diagnosis. While the DoD wrestles with this, there are several steps that a veteran can take. The first is to take a look at the exposure and proof that one has, i.e., DD214, combat records, medical records, etc. The second is to get a brain scan to determine the extent, if any, of damage done to the brain. There are several scans that can be used to do this:
- A Diffusion Tensor Imaging Scan, or DTI
- A Functional Magnetic Resonance Imaging, or fMRI scan
- A Single Photon Emission Computed Tomography (SPECT) Scan can be done by any of the Amen Clinics.
- A Quantitative Encephalogram, or qEEG
These scans can be accomplished by any brain center or hospital, but it’s important that they are read by a neurologist who is knowledgeable of the issue of RBE. Most of these can be found in major cities, and unfortunately, most of these will be out of pocket unless you can convince your VA or Tricare provider to pay for the scan or test. With the right amount of evidence and explanation, you will have a good chance. It is important to note that the CDC has recently declared TBI to be a “chronic” condition, opening up the diagnosis to coverage under Tricare and the VA. The impacts of RBE can be classified as a mTBI, so it is important for the veteran to have that understanding when they appear before the VA or when talking to their physician during their transition. In 2022 the VA also updated billing codes, stating, “the 2023 ICD-10-CM code updates, effective on October 1, 2022, contain a series of codes for ‘S06.8A—Primary blast injury of brain,’ not elsewhere classified.”xii
Treatment: Here is where there can be information overload, but it’s up to the veteran to consult with specialists, their mental health team, or other veterans to determine what set of treatments they should explore to determine how to treat their health. It is not advisable to just start trying many of these treatments, especially psychedelics, without an understanding of what to expect. We can break down treatment into several areas:
- Brain Supplementation and Diets—programs designed based on dietary knowledge and blood tests to identify deficiencies in nutrients and chemicals and to balance brain health with nutraceuticals, vitamins, and minerals.
- Outpatient Procedures—minor surgical procedures like Stellate Ganglion Blocks (SGBs) known to improve brain health.
- Brain Health Treatments—technical modalities designed to stimulate the brain to increase plasticity, stimulation and promote healing. Include a wide range of options from Transcranial Magnetic Stimulation, Hyperbaric Oxygen Treatment, Vagas Nerve Stimulation, Heat/Cold Therapy, Breathing Exercises,
- Psychedelics
- Therapy: there are now modes of therapy that have had amazing effects on veterans but are not approved by the VA. Trauma Resiliency Protocol, Emotions Management Process, and Eye Movement Desensitization and Reprocessing (EMDR) are some of them known to be used by veterans and first responders.
While it is beyond this article to go over every one of the options here (maybe we can run a series), suffice it to say that there are numerous treatment options known to treat and benefit brain health. While there is no “set’ combination of protocols, it is up to the veteran.
This lack of progress on the mental health of veterans, coupled with the continuous prescription of ineffective and mind-numbing drugs, the tragic stories of veteran homicide or suicide, and the never-ending focus on the suicide rate, has created an environment of mistrust and animosity between many veterans and the VA, and that needs to be fixed as we move ahead. We have millions of veterans that have served in the last two wars and millions more that have served before them that have never been assessed for the impact of their careers on their brain health, nor have they been properly treated for any mental illness that they may have displayed as a result of any damage to their brain. These veterans have committed no crime; they signed up to serve their country, and many of them paid for that service with their lives, others with broken bodies, and many, many more with broken brains. We need to lean forward, educate our medical and psychological communities, and make these alternative treatments available to our veterans now.
Endnotes
i. https://missionrollcall.org/veteran-voices/articles/the-state-of-veteran-suicide/ click to return
ii. Neurological Effects of Repeated Blast Exposure in Special Operations Personnel; James R. Stone, Brian B. Avants, Nicholas J. Tustison, Jessica Gill, Elisabeth A. Wilde, Kiel D. Neumann, et.al Journal of Neurotrauma 2024 41:7-8, 942-956 click to return
iii. Impact of repeated blast exposure on active-duty United States Special Operations Forces. Gilmore N, Tseng CJ, Maffei C, Tromly SL, Deary KB, McKinney IR, Kelemen JN, Healy BC, Hu CG et. Al, Proc Natl Acad Sci U S A. 2024 May 7;121(19) click to return
iv. https://neurolaunch.com/blast-brain-injury/ click to return
v. Shively, Sharon Baughman et al. “Characterisation of interface astroglial scarring in the human brain after blast exposure: a post-mortem case series.” The Lancet, Neurology Vol. 15,9 (2016): 944-953. doi:10.1016/S1474- click to return
vi. https://theconversation.com/low-level-blasts-from-heavy-weapons-can-cause-traumatic-brain-injury-2-engineers-explain-the-physics-of-invisible-cell-death-220267 click to return
vii. https://www.research.va.gov/currents/0222-Teasing-out-the-effects-of-blasts-on-mental-health.cfm click to return
viii. https://pmc.ncbi.nlm.nih.gov/articles/PMC9529318/ click to return
ix. https://www.nytimes.com/2023/12/13/us/veterans-weapons-blastexposure.html click to return
x. https://www.ncja.org/crimeandjusticenews/commission-to-study-why-so-many-veterans-end-up-in-jail-prison click to return
1. Rowland JA, Martindale SL. Considerations for the assessment of blast exposure in service members and veterans. Front Neurol. 2024 Apr 15;15:1383710. doi: 10.3389/fneur.2024.1383710. PMID: 38685944; PMCID: PMC11056521.click to return
xii. https://www.research.va.gov/currents/1022-Primary-Blast-Injury-of-the-Brain.cfm click to return

About the Author:
Bruce Parkman entered the Army in 1980 and spent 21 years in the service, including 18 years as a Green Beret serving in the 7th and 10th Special Forces Groups and USAJFKSWCS before retiring as a Sergeant Major in May of 2001. He participated in the El Salvador Conflict as a Combat Advisor and deployed as the Sergeant Major for the 1st (SOCCE) to Kosovo to enforce national policy. In 2020, his son Mac took his life after suffering from undiagnosed mental illness that has been contributed to his extensive exposure to subconcussive trauma from contact sports. To honor his son, he started The Mac Parkman foundation which focuses on the issue of Repetitive Brain Trauma in kids, athletes and veterans and wrote a book called Youth Contact Sports and Broken Brains: Understanding the Hidden Risks of Mental Illness from Early Exposure to Concussive Trauma. He has worked with legislatures, researchers, scientists, parents, doctors and psychologists to spread the work about the risks of subconcussive trauma to make sports safer and to provide improved treatment to veterans.
Mr. Parkman is also the CEO of Blue Fusion Technologies a data integration company and a founding Director of the Green Beret Foundation, Chairman of the Board for the Global Special Operations Forces (SOF) Foundation and remains involved in numerous initiatives to focus on protecting our children.
Leave A Comment